It’s the day after Halloween and we’re already over halfway through induction 2. The previous post was right before he was readmitted for round 2 and we hadn’t had any labs done for over a week so there wasn’t much to report.
On Tuesday, we checked in at 8:30am and got a blood test, a new central line dressing, and spoke with the doctor. There were a few things covered:
In order to start the next round of chemo he needed an ANC (Absolute Neutrophil Count) above 500. We assumed he would be above that, but the last test since he first got home was 400 so we weren’t certain. His count was 750 so he was a go. For reference, a typical ANC is between 1,500 and 8,000; Noah was still neutropenic, just not severely so. His hemoglobin was at 9.6 which had held for the past couple weeks, even if that is still mildly anemic (low end of the typical range is 11). Platelets were all the way up to 340, which is a good range for anyone, as the typical range is 150 to 450.
We got the official results of the MRD (Measurable Residual Disease) testing. In a previous post, I mentioned that the threshold for leukemia was 5 in 10k cells. The testing detected 1 in 10k cells as “abnormal”. Note that this is slightly different than I previously characterized in saying that we don’t know if those 1 in 10k is “not fully developed” vs cancerous. We still don’t know if they are cancer cells, but they are abnormal. So while that’s not as comforting, keep in mind that you and I also have abnormal cells floating around in our bodies; it’s just that a properly working immune system destroys and/or keeps them in check.
There was some question as to whether he would have 4 or 5 rounds of chemo. We got clarification that it would be 5 rounds. As you might imagine, every case is different, and some patients go in with better or worse numbers. Some high-risk factors send a patient down the transplant route almost immediately. Others have relatively better numbers and, if treatment goes well, they only get 4 rounds. At a high-level, Noah’s was something of a middle-ish case; not good, not terrible. 5 stages it is and we hope to not be diverted to the transplant track. We’ll cover more of this as we get to it but, just to prepare, induction 4 is called “Intensification”. Nothing about that word means “easier” unfortunately. But again, let’s focus on the end goal: staying in remission.
On that same theme, they don’t mess around here and Noah’s first treatment was at 4pm on the day of readmission. The protocol for induction 2 is very similar to the first. Every 12 hours he gets either one or two chemo drugs. These drugs are delivered via IV over a period of 20 minutes to an hour. He always receives Cytarabine, which is about a 20 minute drip. On days 1, 3, and 5 the treatment takes about an hour as he additionally gets a heart protectant (Dexrazoxane) treatment preceding a 20 minute drip of Daunorubicin. The Daunorubicin is kind of a sinister looking bright red and poses some risk to the heart. It turns your urine pinkish/orange; really fun stuff. There is a lot of urgency to get that Daunorubicin IV running immediately after the heart protectant to stay within the 30 minute heart protection window.
There are two main differences between induction 1 and 2: First, induction 2 is 8 days instead of 10. Also, on day 6 of induction 1 there was the drug Gemtuzumab, which targets only the “bad” white cells, as opposed to the other drugs that indiscriminately destroy ALL white blood cells. All of this is a bit hand-wavy in that Gemtuzumab technically targets a protein that can be in other types of cells and Cytarabine/Daunorubicin target ANY rapidly dividing cell in the body.
The other drugs are in service of coping with the ill effects of chemo. Nausea and vomiting can creep up without a moment’s notice so there are a number of drugs to assist with that. The first three days of chemo he receives Emend (aprepitant). This is a Pepto-type liquid that, ironically, makes Noah gag. He’s glad when those three doses are done and the medication surely helps him in the coming days. He also gets Zofran (ondansetron) a couple times a day via oral tablet. Benadryl is provided as needed, typically as an option when Zofran won’t be available for a number of hours.
As his counts drop there is a more intensive prevention of bacterial (Levofloxacin) and fungal (Micafungin) infections that the body will be unable to handle itself.
Most of these medications are heavy hitters with their own sets of risks and side effects but, again, this is what we’ve got in 2025.
There are various other meds that are as-needed or may get prescribed based upon how he responds to treatment. For example, his weight got down pretty low last time and Periactin helped to stimulate his appetite. That’s actually an antihistamine but, similar to many drugs, is used off-label for different conditions.
We haven’t been dealing with fevers yet this round, but Tylenol is the typical go-to for that situation. Once his immune system is gone, temperature is monitored closely. Any fever sets off a series of procedures to get the fever down and blood cultures are taken and monitored for infection.
As for what Noah has experienced so far, Wednesday (day 2), Noah was feeling rough with nausea and malaise. We even had to cancel Art class, which is one of his favorites. I kind of assumed he was going to be in for that for a number of days, but he’s really been feeling pretty good these last three days with quite a bit of energy.
Yesterday, we started getting daily labs. This means that blood is drawn via his port at 4am, delivered to the lab, and then we get final counts sometime in the late morning. The doctor typically pops in around 10:30am to answer questions and discuss labs. Labs have been fine to good thus far. When this all started back in early September, Noah’s hemoglobin and platelets both required immediate transfusions and 28% of his white blood cells were leukemia blasts. His numbers were already critical when the first induction started. This time around, he’s starting from a better place. Even four days into treatment his hemoglobin has held at 9.4, platelets have even increased to 370, and ANC moved up to 830.
None of that will hold. In fact, ANC is 500 today which is the threshold of what is considered severe neutropenia. Again, the chemo drugs intend to destroy all white blood cells and will generally suppress bone marrow production. Bone marrow is responsible for producing red and white blood cells and platelets, so all of these will drop and he will get red blood and platelets transfusions eventually. Hopefully it will just be less due to starting from a better place of higher in good counts (hemoglobin and platelets) and lower in bad counts (leukemia cells).
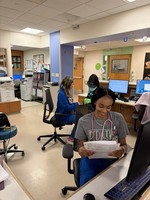
We keep being told “this will be the last day” he can come out of his room, but each morning his ANC has been relatively decent the doctor has let us out for one more day. I’ve got a few pictures below that Mayumi already shared on Facebook, but it was quite the morale boost to be roaming the halls on Halloween. I wasn’t there, but Mayumi said Noah had a marked jolt of joy when the doctor told him he could get out for Halloween. He did some reverse trick-or-treating with the nurses, went to a hospital Halloween party, and had a dance-off with one of the nurses. I saw the video and was a little confused where he picked up those dance moves as Baldwins don’t typically move in a coordinated motion like that.
We’ve tried a little different routine this go-around. Last time Mayumi and I mostly traded nights staying at the hospital every other night. I worked throughout the first induction, save the first week or so, though availability was tricky. Mayumi tends to sleep a lot better at the hospital than I do so she’s staying Monday through Friday and I’ll stay Friday through Monday. During the week, I’ve been coming to the hospital around lunch and then go home around 6:30pm. We’ll see how this works out, but so far, so good.
Noah and I watched the annually required “The Nightmare Before Christmas” yesterday. And then I thought the scary-ish movie “Signs” would be a good Halloween flick. In retrospect, that was probably a bit much for him, but it’s a classic flick. We’ll do another movie night tonight, but likely something a bit more upbeat.
That’s it. Today’s the last day of Daunorubicin. Three more days and we’ll watch the counts come down and then wait for that recovery. We love you all and over and out.